Table of Contents
- Adjustable Gastric Band Late Complications
- Slippage Of The Band
- Erosion Of The Band
- Megaesophagus Or Pseudo Achalasia
- Gastric Bypass Late Complications
- Gallstones
- Marginal Ulcers
- Perforation
- Bowel Obstruction
- Hernia
- Gastric Sleeve Late Complications
- Failing To Lose Weight
- Regaining The Weight Lost
- Intolerance Of Certain Foods
- Malnutrition
- Acid Reflux
- Stomach Ulcers
- Gallstones
- Scarring On The Abdomen
- Hernia
Bariatric surgery has become a popular and effective way to address obesity and weight-related health issues. As you embark on this life-changing procedure, it's essential to be aware of the potential late complications that can occur. Understanding these risks will help you make informed decisions about your health.
In the years following your surgery, you may experience complications related to digestion, nutritional deficiencies, or changes to your gastrointestinal system. Though these complications vary in severity and occurrence, staying vigilant and maintaining open communication with your healthcare team is crucial in managing any arising issues.
It's also important to remember that, despite its benefits, bariatric surgery is not a magic cure for obesity. Adopting and maintaining healthy habits post-surgery is essential to optimize your long-term health outcomes and enjoy a successful weight loss journey.
Adjustable Gastric Band Late Complications
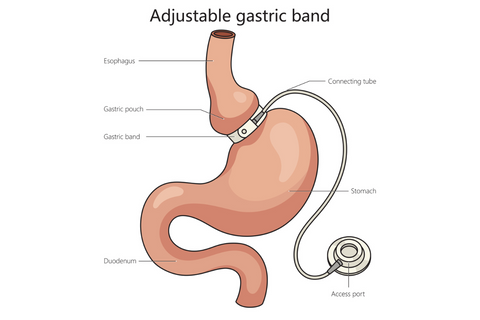
Slippage Of The Band
Slippage of the gastric band is one of the possible late complications after gastric banding surgery. Usually, it occurs months or years after the procedure. It happens when the band slides from its normal position around the stomach, causing the upper part to enlarge. This can lead to heartburn, vomiting, and difficulty swallowing. To correct this issue, your surgeon might need to reposition or even remove the band.
Erosion Of The Band
Another late complication of adjustable gastric banding is band erosion. Over time, the band can wear through the stomach wall, causing it to migrate into the stomach. Erosion of the band increases the risk of severe infection and often leads to a loss of restriction, making you feel less full after eating. In this case, your surgeon will need to remove the eroded band. Depending on your specific situation, an alternative weight loss surgery might be recommended.
Megaesophagus Or Pseudo Achalasia
Megaesophagus, also known as pseudo achalasia, is a severe but rare late complication that can occur years following gastric banding surgery. This condition causes a functional obstruction in the esophagus, leading to difficulty swallowing (dysphagia), regurgitation, and chest pain. To manage this complication, different treatments might be needed, including modifying your eating habits, reversible gastric band deflation, or, in some cases, band removal.
Gastric Bypass Late Complications

Gallstones
After your gastric bypass surgery, you may develop gallstones as a late complication. This occurs due to rapid weight loss, which leads to cholesterol imbalances in your gallbladder. Symptoms include abdominal pain, nausea, and vomiting. Treatment options may involve medication or surgery to remove the gallbladder.
Marginal Ulcers
Marginal ulcers are another potential late complication after gastric bypass surgery, particularly following Roux-en-Y gastric bypass. These ulcers occur at the connection point between your stomach and your small intestine (the anastomosis). Symptoms may include abdominal pain, nausea, and vomiting. To manage this complication, you might require medication or, in severe cases, surgical intervention.
Perforation
Perforation refers to a hole or tears in your gastrointestinal tract. In the context of gastric bypass surgery, this can be a result of anastomotic leaks or ulcers. Symptoms include severe abdominal pain, nausea, and fever. If you experience a perforation, you will need immediate medical attention to repair the damaged tissue.
Bowel Obstruction
A bowel obstruction, a blockage in your gastrointestinal tract, is another possible late complication of gastric bypass surgery. Causes include adhesions (scar tissue) or internal hernias. Symptoms consist of abdominal pain, bloating, and vomiting. To resolve this issue, your healthcare provider may recommend surgery to remove the obstruction.
Hernia
Hernias can develop after gastric bypass surgery, specifically laparoscopic Roux-en-Y procedures. Both internal and incisional hernias may occur. Symptoms include bulging or swelling at the site of the hernia, accompanied by pain and discomfort. Depending on the severity, your doctor will determine if surgical repair is necessary.
Remember to closely monitor your health and consult your healthcare provider if you experience any unusual symptoms following gastric bypass surgery. Early detection and intervention can help address these late complications and improve overall well-being.
Gastric Sleeve Late Complications
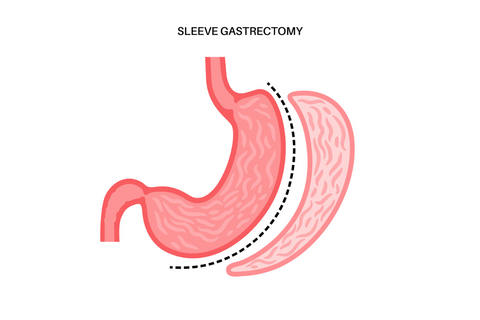
Failing To Lose Weight
In some cases, you may not experience the desired weight loss after a sleeve gastrectomy. Factors like improper diet and insufficient exercise can contribute to inadequate weight loss. It's essential to follow your doctor's guidelines and maintain a healthy lifestyle post-surgery.
Regaining The Weight Lost
The long-term success of gastric sleeve surgery heavily depends on your commitment to a healthy lifestyle. If you don't maintain healthy eating habits and exercise regularly, there's a risk of regaining the lost weight.
Intolerance Of Certain Foods
Your stomach may become more sensitive to certain foods after the surgery. This can lead to nausea, vomiting, and abdominal pain when consuming trigger foods. Pay close attention to your body's reactions and adjust your diet accordingly.
Malnutrition
Since sleeve gastrectomies reduce the size of your stomach, it may impede the absorption of essential nutrients. To prevent malnutrition, make sure to include nutrient-dense foods in your diet and consider taking vitamin and mineral supplements as recommended by your doctor.
Acid Reflux
In some cases, laparoscopic sleeve gastrectomy can lead to gastroesophageal reflux disease (GERD). This occurs when acid in the stomach creeps back into the esophagus, causing heartburn and discomfort. Inform your doctor if you experience these symptoms, as additional treatment may be needed.
Stomach Ulcers
Stomach ulcers may develop after gastric sleeve surgery due to increased stomach acid production. You can minimize the risk of ulcers by avoiding tobacco, alcohol, and NSAIDs, as well as adhering to a prescribed diet plan.
Gallstones
Rapid weight loss following your surgery may increase the risk of gallstone formation. If you experience abdominal pain or other symptoms indicative of gallstones, consult your doctor for appropriate treatment.
Scarring On The Abdomen
While laparoscopic sleeve gastrectomy is minimally invasive, it can still result in scarring on or around the abdominal area. Speak with your doctor about potential scarring and options for minimizing its appearance.
Hernia
In rare cases, a hernia may develop at the site of the surgery. If you experience abdominal pain or a noticeable bulge, seek medical attention promptly.
Also Read: How Can Bariatric Dumping be Prevented (Tips & How to Avoid)



 Order Free Sample
Order Free Sample